Clonal hematopoiesis is characterized by an expansion of blood cells derived from a single mutated hematopoietic stem cell (HSC). When this expansion is driven by a leukemia-associated mutation that exceeds a variant allele frequency (VAF) of 2%, it is termed clonal hematopoiesis of indeterminate potential (CHIP). Approximately half of CHIP cases are driven by mutations in the DNA methyltransferase gene DNMT3A. In patients with CHIP, greater clonal expansion is associated with an increased risk of cardiovascular diseases and hematologic malignancies. While DNMT3A impairment has been shown to alter inflammatory signaling in HSCs and myeloid cells, less is known about the impact of DNMT3A-mutated CHIP on T cell biology. Here, we leverage a cohort of human CHIP samples to assess how the expansion of DNMT3A-mutated cells affects gene expression across blood cell types and generate a new mouse model to assess antigen-specific immune cell interactions. We find evidence that the accumulation of DNMT3A-mutated stem and progenitor cells can cause T cell dysfunction.
We first identified CHIP in a cohort of 191 sternum bone marrow samples collected during heart surgery. We detected CHIP in 45 samples (23.6%), including 22 samples with mutated DNMT3A (48.9% of CHIP samples). To mitigate confounding factors that might be introduced by comparing CHIP to healthy individuals, we used ten DNMT3A-mutated CHIP samples for this study, splitting them into a low-VAF (<10%, three samples) and high-VAF (>10%, seven samples) cohorts. We performed single-cell RNA sequencing on these 10 samples, generating high-quality data for 95,245 cells. We clustered and annotated 33 cell types according to the expression of canonical marker genes, representing the full spectrum of hematopoietic progenitors to myeloid, erythroid and lymphoid lineages.
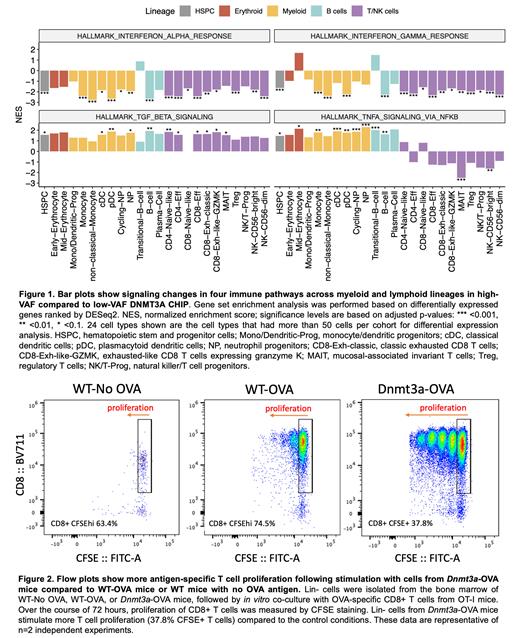
To evaluate how greater DNMT3A clonal expansion affects immune cell states, we performed differential gene expression analysis in the high-VAF compared to the low-VAF cohort with DESeq2 using a pseudobulk approach followed by gene set enrichment analysis using Hallmark pathways. We found that TGF-beta signaling, known for its immunosuppressive role, is upregulated in hematopoietic stem and progenitor cells (HSPCs), myeloid and T cell populations in the high-VAF compared to the low-VAF cohort. Both interferon alpha and gamma signaling pathways are consistently downregulated in HSPCs and multiple myeloid cell types as well as T cells. TNF-alpha signaling is upregulated in HSPCs and myeloid cells, consistent with recent observations linking TNF-alpha to the survival and proliferation of HSPCs and myeloid cells. Overall, greater expansion of DNMT3A-mutated cells is associated with variable gene expression changes in progenitor and myeloid cell types, whereas gene expression changes in T cells are consistent with diminished activation (Figure 1).
To evaluate mechanisms contributing to altered T cell activation in DNMT3A-mutated CHIP, we combined our Dnmt3a-fl-R878H/+ inducible mouse model with the ovalbumin (OVA) trackable antigen system. Endogenously expressed OVA is processed into a peptide that is loaded onto MHCI and recognized by transgenic CD8+ T cells from OT-I mice. We crossed the Dnmt3a-fl-R878H/+ mouse with a mouse expressing OVA under the actin promoter, resulting in Dnmt3a-mutated mice with constitutive OVA expression. To interrogate antigen-specific T cell responses, we co-cultured Dnmt3a-mutated OVA+ lineage negative (Lin-) stem and progenitor cells with CD8+ T cells from OT-I mice. By measuring T cell proliferation using CFSE dilution, we observed an increase in T cell proliferation when CD8+ T cells were co-cultured with Dnmt3a-mutated OVA+ Lin- cells compared to wildtype OVA+ Lin- cells (Figure 2). These results suggest that Lin- Dnmt3a-mutated cells have an increased capacity for antigen-specific T cell activation.
In conclusion, our studies demonstrate that greater expansion of DNMT3A-mutated CHIP is associated with reduced expression of activation signatures in T cells. In apparent contrast, Dnmt3a-mutated mouse cells have an increased capacity for antigen-specific T cell stimulation. Since chronic antigenic stimulation causes T cell exhaustion, our findings are consistent with a model in which the expansion of DNMT3A-mutated progenitor and myeloid cells causes chronic stimulation and dysfunction of T cells.
Disclosures
Sperling:Novartis: Consultancy; Roche: Consultancy. Bick:TenSixteen Bio: Membership on an entity's Board of Directors or advisory committees. Trowbridge:H3 Biomedicine, Inc: Research Funding; Fate Therapeutics: Patents & Royalties. van Galen:Immunitas: Consultancy; ManaT Bio: Consultancy.